2022.PE
(→病例详细描述) |
(→全血细胞计数和血液化学解释) |
||
| 第94行: | 第94行: | ||
在第一次全血细胞计数 '''10 小时后'''获得第二次全血细胞计数'''显示贫血'''证据(红细胞 4.31 × 10^12/l,参考范围:5.65-8.87 × 1012/l;Hct 26.8%,参考范围:37.3%–61.7%;Hgb 9.5 g/dl,参考范围:13.1-20.5 g/dl),'''白细胞增加'''(17.6 × 10^9/l,参考范围:6-16.9 × 10^9/l)和分段中性粒细胞(15.19×10^9/l,参考范围:2.8-10.5 × 10^9/l)。'''PLT低于前一个''',低于参考范围:116×10^9/l(参考范围:175-500×10^9/l)。大约 12 小时后进行第三次全血细胞计数第二个显示红细胞进一步下降(高达3.36×10^12/l参考范围:5.65-8.87×10^12/l Hct 20.2%,参考范围:37.3%-61.7%;Hgb 7.4 g/dl,参考范围:13.1-20.5 g/dl)。PLT和WBC与之前的血液检查相比没有变化。总胆红素 (28 mg/dl) 和血清尿素 (25 mg/dl) 增加(参考范围:分别为 7-25 mg/dl 和 8.6-11.8 mg/dl)。所有数据均在表1中报告。收集胸腔积液样本进行培养和药敏试验,以及细胞学评估。'''胸腔积液'''的细胞学检查和从提交的液体制备的浓缩样本的细胞学检查显示细胞浓度低,'''有明显的血液稀释'''。大多数有核细胞是巨噬细胞,这些细胞通常是空泡化的,并含有吞噬细胞化的细胞物质。观察到反应性间皮细胞数量较少。未发现传染性生物体或明显的非典型细胞群。中性粒细胞与血液稀释程度相容。有既往出血(吞噬红细胞)的证据,但在胸腔积液细胞学检查中不明显有明显的炎症(心包炎)。 | 在第一次全血细胞计数 '''10 小时后'''获得第二次全血细胞计数'''显示贫血'''证据(红细胞 4.31 × 10^12/l,参考范围:5.65-8.87 × 1012/l;Hct 26.8%,参考范围:37.3%–61.7%;Hgb 9.5 g/dl,参考范围:13.1-20.5 g/dl),'''白细胞增加'''(17.6 × 10^9/l,参考范围:6-16.9 × 10^9/l)和分段中性粒细胞(15.19×10^9/l,参考范围:2.8-10.5 × 10^9/l)。'''PLT低于前一个''',低于参考范围:116×10^9/l(参考范围:175-500×10^9/l)。大约 12 小时后进行第三次全血细胞计数第二个显示红细胞进一步下降(高达3.36×10^12/l参考范围:5.65-8.87×10^12/l Hct 20.2%,参考范围:37.3%-61.7%;Hgb 7.4 g/dl,参考范围:13.1-20.5 g/dl)。PLT和WBC与之前的血液检查相比没有变化。总胆红素 (28 mg/dl) 和血清尿素 (25 mg/dl) 增加(参考范围:分别为 7-25 mg/dl 和 8.6-11.8 mg/dl)。所有数据均在表1中报告。收集胸腔积液样本进行培养和药敏试验,以及细胞学评估。'''胸腔积液'''的细胞学检查和从提交的液体制备的浓缩样本的细胞学检查显示细胞浓度低,'''有明显的血液稀释'''。大多数有核细胞是巨噬细胞,这些细胞通常是空泡化的,并含有吞噬细胞化的细胞物质。观察到反应性间皮细胞数量较少。未发现传染性生物体或明显的非典型细胞群。中性粒细胞与血液稀释程度相容。有既往出血(吞噬红细胞)的证据,但在胸腔积液细胞学检查中不明显有明显的炎症(心包炎)。 | ||
| + | |||
| + | |||
| + | A coagulation profile was completed and showed severe prolongation of prothrombin and partial thromboplastin time (PTT) PT (prothrombin time 100 seconds, reference range: 11–17 seconds; and PPT 128 seconds, reference range: 12–16 seconds) (Valchev et al., 2008). Cardiac troponin I was within normal ranges (0.01 ng/ml, reference range: <0.06 ng/ml). | ||
| + | |||
| + | 完成凝血曲线并显示凝血酶原和部分凝血活酶时间 (PTT) PT 的严重延长(凝血酶原时间 100 秒,参考范围:11-17 秒;PPT 128 秒,参考范围:12-16 秒)(Valchev 等人,2008 年)。心肌肌钙蛋白I在正常范围内(0.01 ng/ml,参考范围:<0.06 ng/ml)。 | ||
| + | |||
| + | |||
| + | The patient was hospitalized overnight with IV fluid therapy and was started on amoxicillin-clavulanic acid (25 mg/kg every 12 hours PO – Synulox, Zoetis) and vitamin K (5 mg/kg every 12 hours IV; Vitamin K1 Laboratoire TVM, Domes Pharma). | ||
| + | |||
| + | 患者住院过夜接受静脉输液治疗,并开始使用阿莫西林-克拉维酸(25 mg/kg,每 12 小时 PO – Synulox、Zoetis)和维生素 K(5 mg/kg,每 12 小时静脉注射;维生素 K1 实验室 TVM,Domes Pharma)。 | ||
| + | |||
| + | |||
| + | A CT examination, follow-up echocardiography, and possible pericardiocentesis in case of cardiac tamponade were planned for the next day. The next morning the patient was bright, alert, and responsive. She ate normally during the night. The mucous membrane refill time was within normal ranges and the jugular pulses were normal. Temperature was 39.7°C. The heart rate was 180 beats per minute and heart sounds were not muffled. Femoral pulses were strong. Pulmonary auscultation was unremarkable and the previous respiratory signs had resolved. Already after the first IV vitamin K supplementation, PT/PTT returned within normal limits. Oscillometric blood pressure evaluation was within normal limits | ||
| + | |||
| + | 计划在第二天进行 CT 检查、随访超声心动图和心包穿刺术(如果发生心包填塞)。第二天早上,病人神采奕奕,神志清醒,反应灵敏。她晚上吃得很正常。黏膜再充盈时间在正常范围内,颈静脉搏动正常。温度为39.7°C。 心率为每分钟180次,心音没有减弱。股动脉搏动很强。肺部听诊无明显异常,既往呼吸系统体征已消退。在第一次静脉注射维生素 K 后,PT/PTT 恢复到正常范围内。示波血压评估在正常范围内 | ||
<br> | <br> | ||
2024年6月16日 (日) 16:07的版本
目录 |
1 摘要
An adult mixed-breed dog was presented for 1-day history of anorexia and cough. Thoracic radiographs revealed moderate generalized cardiomegaly with globoid-shaped cardiac silhouette and mild bilateral pleural effusion.
一只成年混种犬因厌食和咳嗽 1 天病史而就诊。胸片显示中度全身性心脏扩大,伴有球状心脏轮廓和轻度双侧胸腔积液。
Echocardiography showed mild tamponating pericardial effusion and diffuse severe thickened pericardium.
超声心动图显示轻度心包积液和弥漫性重度心包增厚。
Complete blood count and blood chemistry at presentation were not specific.
就诊时的全血细胞计数和血化成分不具有特异性。
A coagulation profile was completed and showed severe prolongation of prothrombin time and partial thromboplastin time.
完成凝血功能检查,显示凝血酶原时间和部分凝血活酶时间严重延长。
Intravenous therapy with vitamin K was started at 5mg/kg BID and on follow-up echocardiography performed 12 hours later there was evidence of complete regression of the pericardial thickening and pericardial effusion.
以 5mg/kg BID 开始静脉注射维生素 K 治疗,12 小时后进行随访超声心动图检查,有证据表明心包增厚和心包积液完全消退。
To the authors' knowledge, this is the first case report describing severe pericardial thickening, constrictive pericarditis, and cardiac tamponade secondary to spontaneous anticoagulant-induced hemopericardium in dogs.
据作者所知,这是第一份描述严重心包增厚、缩窄的病例报告狗自发性抗凝血诱发的心包炎和心包填塞。
Pericardial effusions are well described in dogs; however, their association with rodenticide intoxication in the canine population is not widely described.
心包积液在狗中得到了很好的描述;然而,它们与犬类种群中杀鼠剂中毒的关联尚未得到广泛描述。
2 病例详细描述
A 2-year-old female indoor spayed mixed-breed dog was initially presented to her veterinarian for a 1-day history of anorexia and cough. The owners did not report history of exposure to rodenticides. The dog presented muffled heart sounds and thoracic radiographs revealed moderate globoid enlargement of the cardiac silhouette [vertebral heart score (VHS) of approx. 13], mild bilateral pleural effusion, and mild retraction of the lung lobes. Complete blood count (CBC) and chemistry panel at presentation were unremarkable [red blood count (RBC) 6.1 ×1012/l, reference range: 5.65–8.87×1012/l; Hct 39.4%, reference range: 37.3%–61.7%; Hgb 16.3 g/dl, reference range: 13.1–20.5 g/dl; white blood count (WBC) 11.7 × 109/l, reference range: 6–16.9×109/l; and segmented neutrophils 7.4 × 109/l, reference range: 2.8–10.5 × 109/l]. Platelet count (PLT) was within normal limits at 212 × 109 /l (reference range: 175–500 × 109/l). The chemistry panel revealed mild hyperglycemia (145 mg/dl, reference range: 60–110mg/dl), mild hypoalbuminemia 2.4 g/dl (reference range: 2.5–4.4 g/dl) and hypoglobulinemia 1.7 g/dl (reference range: 2.3–5.2 g/dl). CBC and chemistry data at presentation are reported in Table 1.
一只 2 岁的雌性室内绝育混种狗最初因厌食和咳嗽 1 天病史而被送往兽医处。业主没有报告接触杀鼠剂的历史。这只狗表现出低沉的心音,胸片显示心脏轮廓中度球状肿大 [椎体心脏评分 (VHS) 约为 13],轻度双侧胸腔积液和肺叶轻度回缩。就诊时全血细胞计数 (CBC) 和生化检查无明显异常 [红细胞计数 (RBC) 6.1 ×1012/l,参考范围:5.65–8.87×1012/l;Hct 39.4%,参考范围:37.3%–61.7%;Hgb 16.3 g/dl,参考范围:13.1–20.5 g/dl;白细胞计数 (WBC) 11.7 × 10^9/l,参考范围:6–16.9×10^9/l;和分段中性粒细胞 7.4 × 10^9/L,参考范围:2.8–10.5 × 10^9/l]。血小板计数 (PLT) 在 212 × 10^9 /l 时在正常范围内(参考范围:175-500 × 10^9/l)。生化检查显示轻度高血糖(145 mg/dl,参考范围:60-110mg/dl)、轻度低白蛋白血症 2.4 g/dl(参考范围:2.5-4.4 g/dl)和低球蛋白血症 1.7 g/dl(参考范围:2.3-5.2 g/dl)。表1报告了就诊时的全血细胞计数和化学数据。
The patient was referred to an emergency and specialty center for further evaluation. On presentation to the referral center that same day, the patient was reported to have a temperature of 37.4°C. On initial examination, the dog was tachycardic (heart rate 160 bpm), with cyanotic mucous membrane and prolonged refill time (>2 seconds). The patient had abnormal jugular pulses. Cardiac auscultation revealed mildly muffled heart sounds with regular rhythm. Respiratory rate was 34 breaths per minute. Oscillometric blood pressure evaluation was lower than normal limits (systolic pressure average of 100 mmHg). The QRS complexes were attenuated and electrical alternans was appreciated. Thoracic point of care ultrasound confirmed the presence of pericardial and pleural effusion. A complete echocardiographic examination demonstrated the presence of severe pericardial thickening, mild pericardial effusion, mild pleural effusion, and hemodynamic changes consistent with constrictive pericarditis (CP). Computed tomography (CT) was scheduled to further characterize cardiac abnormalities and for presurgical pericardiectomy planning.
患者被转诊至急诊和专科中心进行进一步评估。当日到转诊中心就诊时,病人体温为37.4°C。 初步检查时,狗有心动过速(心率 160 次/分),粘膜发绀,再充盈时间延长(>2 秒)。患者颈静脉搏动异常。 心脏听诊显示心音轻度低沉,心律规律。呼吸频率为每分钟 34 次。示波血压评估低于正常限值(收缩压平均值为 100 mmHg)。QRS波群衰减,电交替物受到赞赏。胸部床旁超声证实存在心包积液和胸腔积液。完整的超声心动图检查显示存在重度心包增厚、轻度心包积液、轻度胸腔积液和符合缩窄性心包炎 (constrictive pericarditis, CP) 的血流动力学改变。计划进行计算机断层扫描 (CT) 以进一步表征心脏异常和术前心包切除术计划。
3 胸片解读 (Thoracic radiographs interpretation)
就诊时的胸片显示气管抬高,与脊柱平行。心脏轮廓适度扩大,胸骨接触宽阔,球状,边缘清晰(VHS约13)。有轻度双侧胸腔积液和肺叶轻度回缩。颅腹肺叶显示轻度弥漫性非结构性混浊增加,与间质-肺槽肺模式相符,很可能与回缩和轻度肺不张有关。影像学检查结果与心包积液相符,伴有心包填塞和右心衰竭的体征。
Thoracic radiographs at presentation showed elevation of the trachea which was parallel to the spine. The cardiac silhouette was moderately enlarged, with a broad sternal contact, a globoid shape and sharply defined margins (VHS approx. 13). There was mild bilateral pleural effusion and mild retraction of the lung lobes. The cranioventral lung lobes showed mild diffuse unstructured increase in opacity compatible with an interstitio-toalveolar lung pattern, most likely related to retraction and mild atelectasis. Radiographic findings were compatible with pericardial effusion with signs of cardiac tamponade and right-sided heart failure.
4 超声心动图解读 (Echocardiogram interpretation)
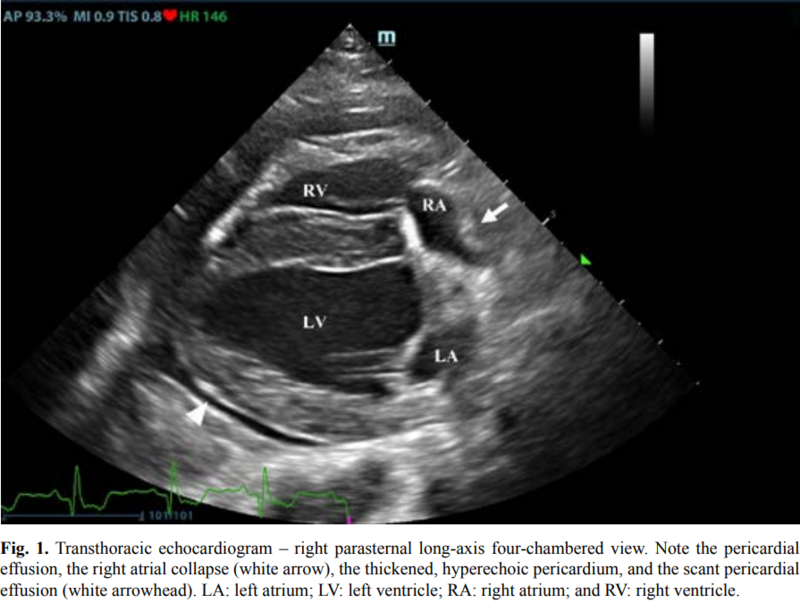
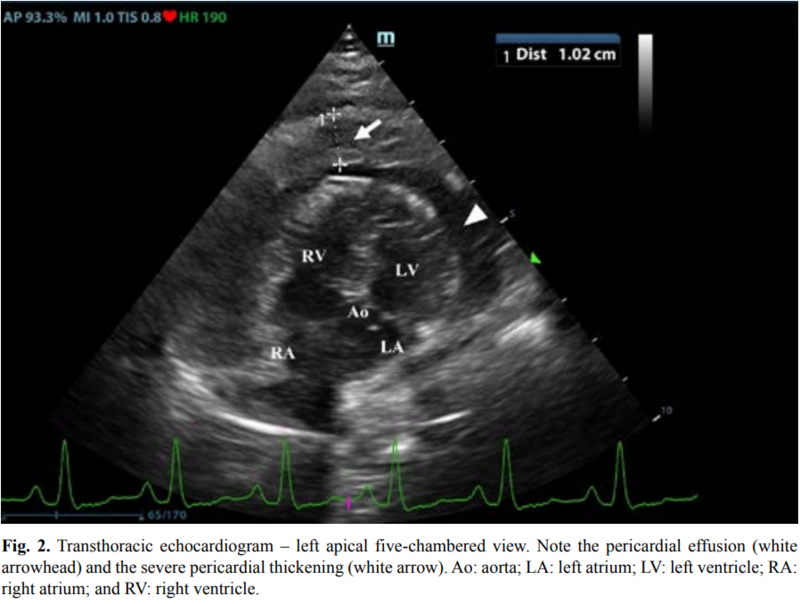
First, transthoracic echocardiogram findings were a small amount of circumferential tamponating pericardial effusion (Fig. 1) and a severe hyperechoic pericardial thickening (10.2 mm) (Fig. 2). The right atrium was normal in size and there was collapse during systole.
首先,经胸超声心动图发现少量环形填孔性心包积液(图 1)和严重的高回声心包增厚 (10.2 mm)(图 2)。右心房大小正常,收缩期有塌陷。
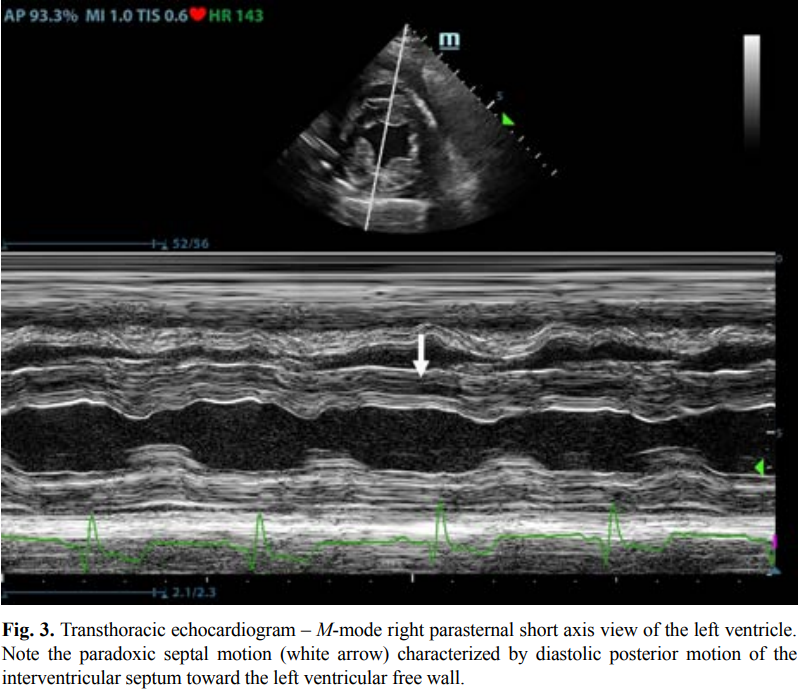
There was mild septal flattening seen on short axis view of the left ventricle. A short-axis left ventricular M-mode showed posterior displacement of the interventricular septum during late diastole at the time of atrial systole (Fig. 3). The epicardium and pericardium had a hyperechoic appearance with a thin, shaggy layer of heterogeneous echogenic material lining the surface of each (Fig. 1, Supplementary Video I).
左心室短轴位可见轻度间隔扁平。短轴左心室 M 型显示心房收缩期晚期舒张期室间隔向后移位(图 3)。心外膜和心包具有高回声外观,每个表面都有一层薄而毛茸茸的异质回声物质(图 1,补充视频 I)。
Pericardiocentesis was not recommended at this time given that the patient was minimally clinically and hemodynamically affected. Few hours later, a second echocardiographic examination, after stabilization of left ventricular volume with intravenous (IV) lactate ringer solution at maintenance rate, showed a worsening of pericardial thickness (13mm) and an increase in pleural effusion.
鉴于患者的临床和血流动力学影响最小,目前不建议进行心包穿刺术。几小时后,在左心室容积稳定后,第二次超声心动图检查显示心包厚度 (13mm) 恶化,胸腔积液增加。
Furthermore, there was a >25% mitral inflow variation noted with respiration. In addition, there was >30% tricuspid inflow variation with respiration, signs of CP. During the second echocardiography, the patient appeared to be slightly dyspneic due to the increased thoracic effusion.
此外,呼吸时二尖瓣流入变化>25%。此外,有>30%的三尖瓣流入变化随呼吸,有CP的体征。在第二次超声心动图检查中,由于胸腔积液增加,患者似乎有轻微的呼吸困难。
5 全血细胞计数和血液化学解释
CBC and blood chemistry interpretation
A second CBC obtained 10 hours after the first one showed evidence of anemia (RBC 4.31 × 1012/l, reference range: 5.65–8.87 × 1012/l; Hct 26.8%, reference range: 37.3%–61.7%; and Hgb 9.5 g/dl, reference range: 13.1–20.5 g/dl), an increased WBC (17.6 × 109/l, reference range: 6–16.9 × 109/l), and segmented neutrophils (15.19× 109/l, reference range: 2.8–10.5 × 109/l). PLT was lower than the previous one and lower compared to the reference ranges: 116 × 109/l (reference range: 175–500× 109/l). A third CBC performed about 12 hours after the second one showed further decrease in the RBC (up to 3.36 × 1012/l reference range: 5.65–8.87 × 1012/l Hct 20.2%, reference range: 37.3%–61.7%; and Hgb 7.4 g/dl, reference range: 13.1–20.5 g/dl). PLT and WBC were unchanged compared to the previous blood work. Total bilirubin (28 mg/dl) and serum urea (25 mg/dl) increased (reference ranges: 7–25 mg/dl and 8.6–11.8 mg/dl, respectively). All data are reported in Table 1. A sample of pleural effusion was collected for culture and susceptibility testing, as well as cytologic evaluation. Cytology of the pleural fluid and a concentrated sample prepared from submitted fluid were of low cellularity with marked hemodilution. Most nucleated cells were macrophages, and these were often vacuolated and contained phagocytized cellular material. Low numbers of reactive mesothelial cells were seen. No infectious organisms or overtly atypical cell populations were found. Neutrophils were compatible with the degree of hemodilution. There was evidence of prior hemorrhage (phagocytized erythrocytes), but significant inflammation (pericarditis) was not apparent in the cytology of the pleural fluid.
在第一次全血细胞计数 10 小时后获得第二次全血细胞计数显示贫血证据(红细胞 4.31 × 10^12/l,参考范围:5.65-8.87 × 1012/l;Hct 26.8%,参考范围:37.3%–61.7%;Hgb 9.5 g/dl,参考范围:13.1-20.5 g/dl),白细胞增加(17.6 × 10^9/l,参考范围:6-16.9 × 10^9/l)和分段中性粒细胞(15.19×10^9/l,参考范围:2.8-10.5 × 10^9/l)。PLT低于前一个,低于参考范围:116×10^9/l(参考范围:175-500×10^9/l)。大约 12 小时后进行第三次全血细胞计数第二个显示红细胞进一步下降(高达3.36×10^12/l参考范围:5.65-8.87×10^12/l Hct 20.2%,参考范围:37.3%-61.7%;Hgb 7.4 g/dl,参考范围:13.1-20.5 g/dl)。PLT和WBC与之前的血液检查相比没有变化。总胆红素 (28 mg/dl) 和血清尿素 (25 mg/dl) 增加(参考范围:分别为 7-25 mg/dl 和 8.6-11.8 mg/dl)。所有数据均在表1中报告。收集胸腔积液样本进行培养和药敏试验,以及细胞学评估。胸腔积液的细胞学检查和从提交的液体制备的浓缩样本的细胞学检查显示细胞浓度低,有明显的血液稀释。大多数有核细胞是巨噬细胞,这些细胞通常是空泡化的,并含有吞噬细胞化的细胞物质。观察到反应性间皮细胞数量较少。未发现传染性生物体或明显的非典型细胞群。中性粒细胞与血液稀释程度相容。有既往出血(吞噬红细胞)的证据,但在胸腔积液细胞学检查中不明显有明显的炎症(心包炎)。
A coagulation profile was completed and showed severe prolongation of prothrombin and partial thromboplastin time (PTT) PT (prothrombin time 100 seconds, reference range: 11–17 seconds; and PPT 128 seconds, reference range: 12–16 seconds) (Valchev et al., 2008). Cardiac troponin I was within normal ranges (0.01 ng/ml, reference range: <0.06 ng/ml).
完成凝血曲线并显示凝血酶原和部分凝血活酶时间 (PTT) PT 的严重延长(凝血酶原时间 100 秒,参考范围:11-17 秒;PPT 128 秒,参考范围:12-16 秒)(Valchev 等人,2008 年)。心肌肌钙蛋白I在正常范围内(0.01 ng/ml,参考范围:<0.06 ng/ml)。
The patient was hospitalized overnight with IV fluid therapy and was started on amoxicillin-clavulanic acid (25 mg/kg every 12 hours PO – Synulox, Zoetis) and vitamin K (5 mg/kg every 12 hours IV; Vitamin K1 Laboratoire TVM, Domes Pharma).
患者住院过夜接受静脉输液治疗,并开始使用阿莫西林-克拉维酸(25 mg/kg,每 12 小时 PO – Synulox、Zoetis)和维生素 K(5 mg/kg,每 12 小时静脉注射;维生素 K1 实验室 TVM,Domes Pharma)。
A CT examination, follow-up echocardiography, and possible pericardiocentesis in case of cardiac tamponade were planned for the next day. The next morning the patient was bright, alert, and responsive. She ate normally during the night. The mucous membrane refill time was within normal ranges and the jugular pulses were normal. Temperature was 39.7°C. The heart rate was 180 beats per minute and heart sounds were not muffled. Femoral pulses were strong. Pulmonary auscultation was unremarkable and the previous respiratory signs had resolved. Already after the first IV vitamin K supplementation, PT/PTT returned within normal limits. Oscillometric blood pressure evaluation was within normal limits
计划在第二天进行 CT 检查、随访超声心动图和心包穿刺术(如果发生心包填塞)。第二天早上,病人神采奕奕,神志清醒,反应灵敏。她晚上吃得很正常。黏膜再充盈时间在正常范围内,颈静脉搏动正常。温度为39.7°C。 心率为每分钟180次,心音没有减弱。股动脉搏动很强。肺部听诊无明显异常,既往呼吸系统体征已消退。在第一次静脉注射维生素 K 后,PT/PTT 恢复到正常范围内。示波血压评估在正常范围内